Credit Photo by Caroline Selfors on Unsplash
Over the past year, many of you have joined us on a voyage of rare disease discovery. We have shared the huge challenges facing the rare disease community – from patients and their carers, clinicians and the companies developing life-saving treatments for patients in need.
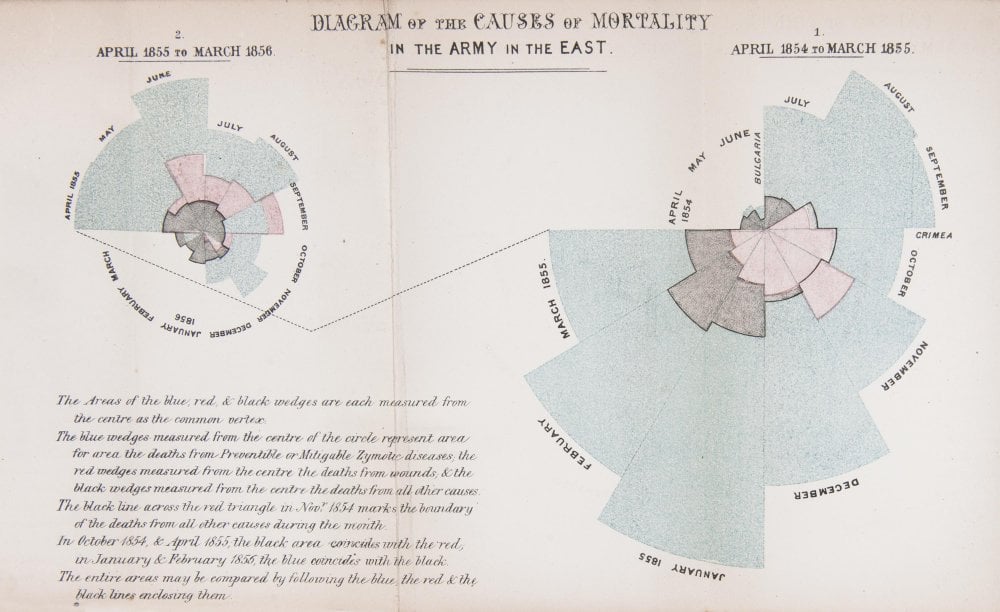
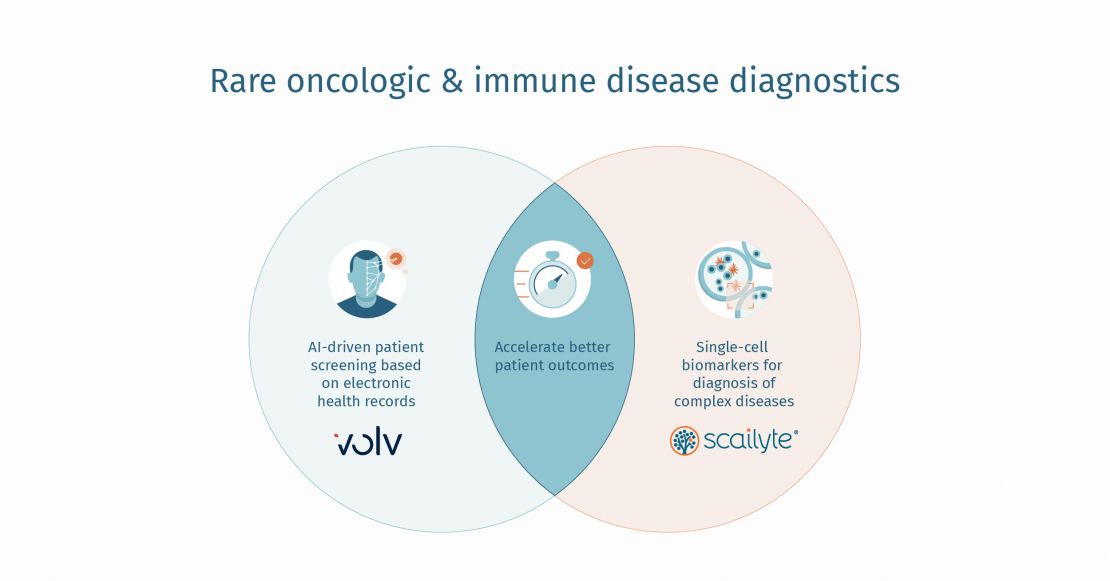
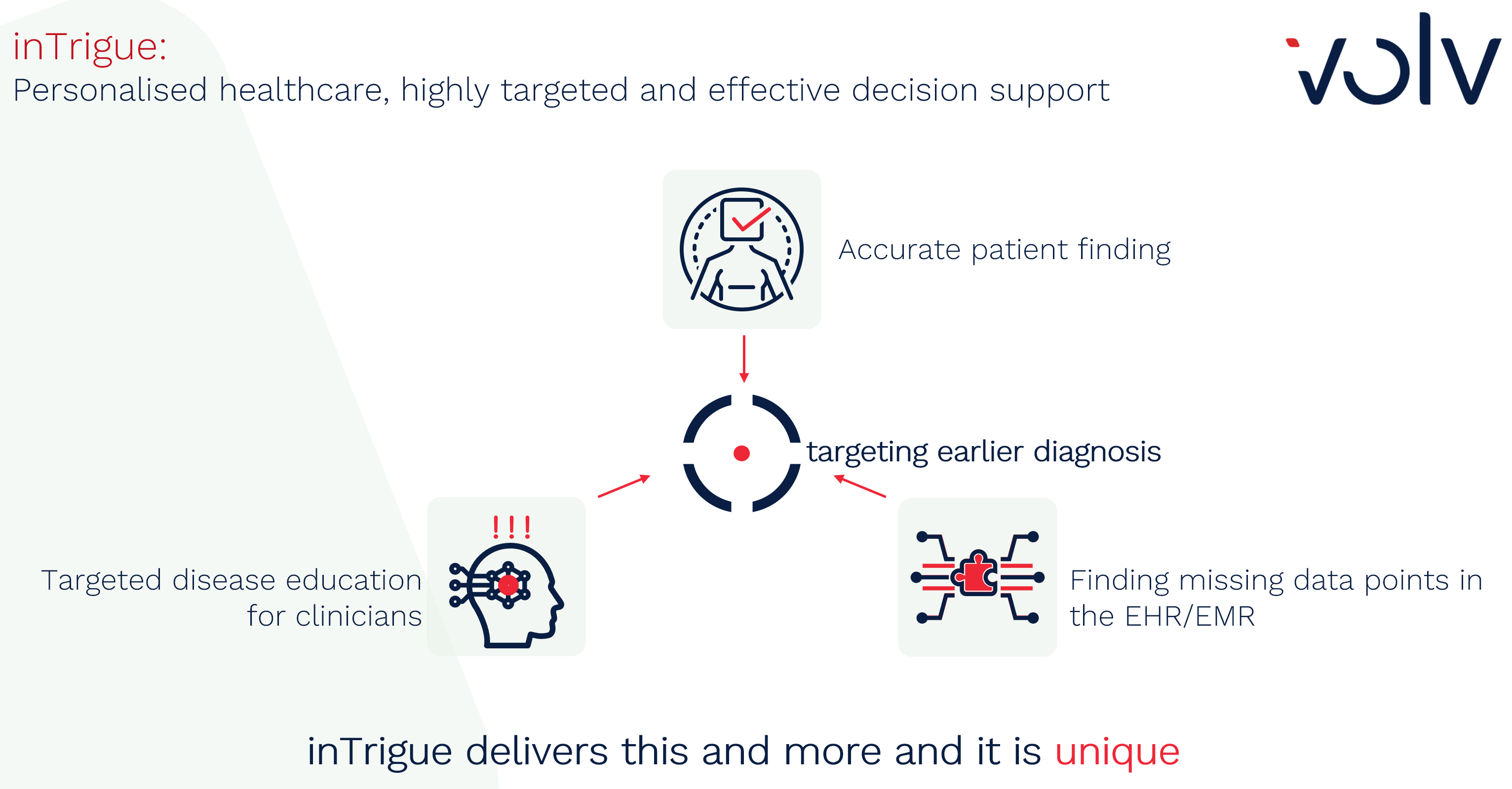
How those challenges are framed varies depending on the stakeholder, but they boil down to the same issue: searching for, accurately identifying, diagnosing, and treating patients with rare and ultra-rare diseases. The difficulty is compounded by the fact that there are as many as 9,332 unique rare diseases and 21,582 synonyms, according to data from Orphanet.
We have described the ability to pick out patterns to identify patients with rare diseases as being a bit like identifying thousands of constellations of stars: Neither is within the scope of the human eye and both require extremely advanced technologies to even begin to decipher and separate patterns.
Yet to research and develop innovative products for rare diseases, companies must find ways to identify populations of patients for study purposes. And as the millions of patients with rare diseases and their families know all-too-well, the wait for a diagnosis, much less treatment, can be painfully slow, with symptoms often missed or not well-understood by the doctors that they see. Over the summer, we have shared real-world stories with you from patients with rare diseases and conditions or from the parents of children with debilitating rare diseases.
We shared Paul’s battle to get his narcolepsy recognised, diagnosed, and treated and the huge battle he faced professionally and medically. Tamsyn shared her difficult journey with getting the recognition, treatment and support she needed for her rare condition, Poland Syndrome, and how the poor understanding of her condition by healthcare professionals led her to studying biological sciences at university and to her passion for work in the rare disease space. And Bernd shared his story as a parent of a child with Alström syndrome and his battle to get his son, Ben, the support he needs.
Download the Presentation here:







.jpg)